A Mouth Sore That Won’t Heal? A sore spot in your mouth can be easy to ignore. Maybe you bit your cheek, burned your tongue, or chewed too aggressively. It hurts a little, then fades—usually. But when that sore lingers longer than two weeks, doesn’t fade, or seems to be worsening, it’s time to pause and take it seriously. A persistent mouth sore may be the earliest warning sign of something deeper.
In this comprehensive guide, we’ll unpack everything you need to know about mouth sores that won’t heal. You’ll understand what causes them, what they look like, when to worry, what a dentist or oral specialist will do, and most importantly—what steps can protect your long-term oral and overall health.
The Anatomy of a Mouth Sore: More Than Just Irritation
Your oral mucosa—the soft lining inside your cheeks, gums, tongue, and lips—is designed to heal rapidly. It’s one of the fastest-regenerating tissues in the human body. Most minor injuries, like a cheek bite or pizza burn, start to resolve within 7–10 days.
But a non-healing oral ulcer—one that stays raw, painful, white or red, or starts to change shape—signals that something is preventing proper healing. This may be due to ongoing trauma, infection, inflammation, or in rare but critical cases, a precancerous or cancerous lesion.
Many people are surprised to learn that most persistent oral sores are not caused by cancer, but that doesn’t make them benign. Repeated irritation from a sharp tooth edge, broken filling, or poorly fitting denture can cause a gum lesion or cheek ulcer. If the source of trauma isn’t corrected, the tissue remains inflamed and can begin to change.
What Causes a Mouth Sore That Doesn’t Go Away?
Conditions like oral candidiasis (thrush) or herpes simplex virus can create ulcerations that persist or recur. Immunocompromised patients are especially prone to these infections.
Certain systemic diseases such as lichen planus, pemphigus vulgaris, and lupus can cause recurrent or chronic oral ulcers. These conditions require a dental soft tissue exam along with coordination between your dentist and physician.
Lack of iron, folate, or vitamin B12 may impair tissue repair and cause sore-like lesions. These can resemble precancerous mouth lesions, and blood work is often needed to confirm the underlying cause.
A persistent sore could be a symptom of oral squamous cell carcinoma, especially if accompanied by weight loss, hoarseness, or a white patch in the mouth that thickens or bleeds. This is where early detection becomes critical.
Here’s a concise list of common causes of mouth sores that don’t heal, based on your article:
- Chronic trauma – from sharp teeth, broken fillings, or poorly fitting dentures
- Fungal infections – like oral candidiasis (thrush)
- Viral infections – such as herpes simplex virus (HSV)
- Autoimmune diseases – including lichen planus, lupus, and pemphigus vulgaris
- Nutritional deficiencies – particularly in iron, vitamin B12, or folate
- Immunosuppression – due to conditions like HIV or cancer treatment
- Tobacco and alcohol use – which irritate the oral tissues and slow healing
- Pre-cancerous changes – such as leukoplakia or erythroplakia
- Oral cancer – especially squamous cell carcinoma
- Poor oral hygiene – which increases the risk of infections and delayed healing
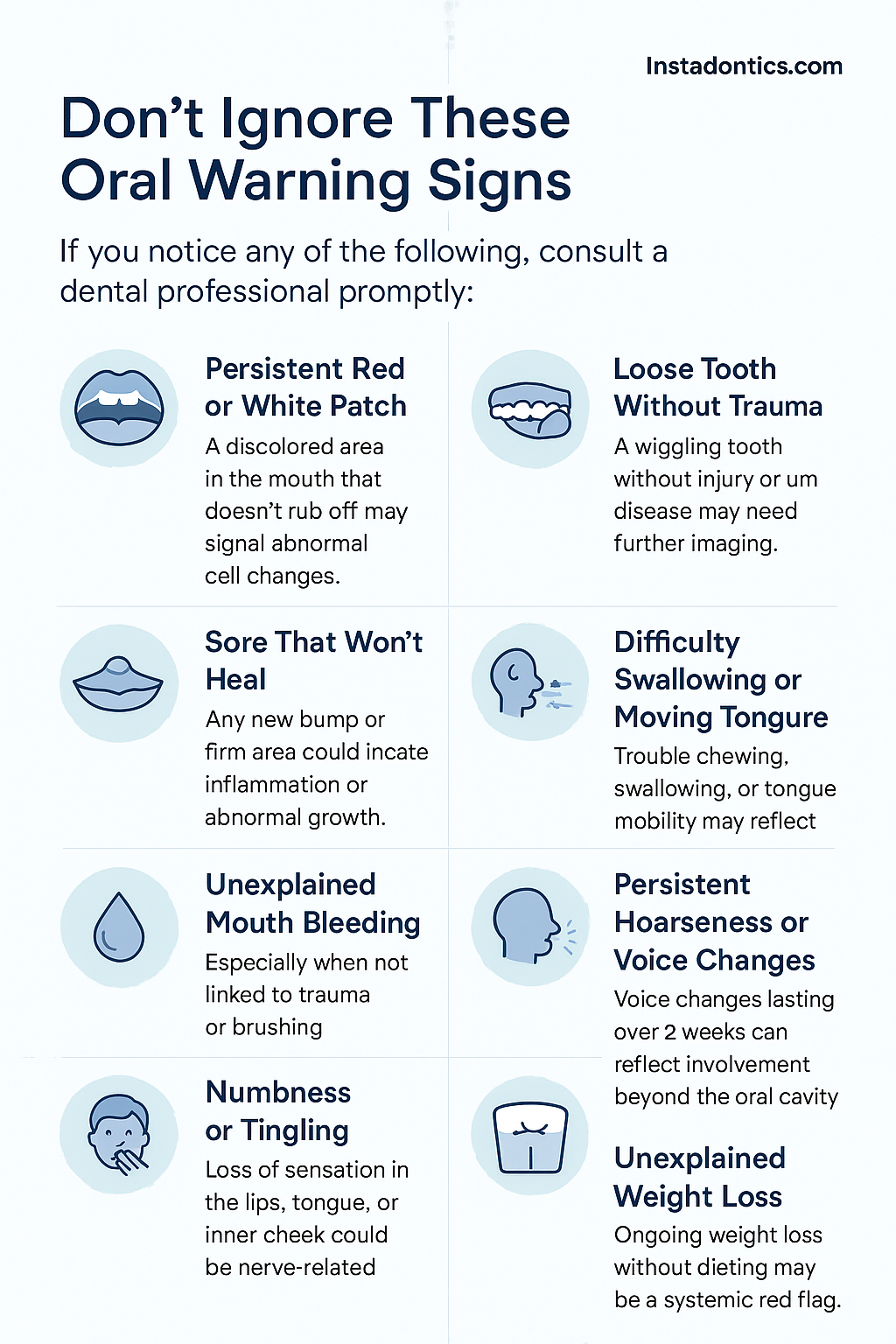
When to Be Concerned: Red Flags of Oral Cancer
Many patients delay seeing a dentist because their sore doesn’t hurt. But oral cancer signs are often painless in the early stages.
A white or red patch that doesn’t rub off is a concerning sign. So is a sore on the tongue or floor of the mouth that hasn’t healed in over 14 days. A lump, bump, or area of thickened tissue also warrants immediate attention.
Unexplained bleeding, numbness or tingling in a localized area, loose teeth, changes in denture fit, or difficulty swallowing, chewing, or moving the tongue can all point to underlying pathology. These symptoms don’t always mean cancer—but they do warrant a professional oral health screening and possibly an oral biopsy to rule out serious conditions.
Here’s a clean, clear list of red flags for oral cancer based on the “When to Be Concerned” section of your article:
🚩 Red Flags of Oral Cancer
If you notice any of the following, consult a dental professional promptly:
- A white or red patch in the mouth that does not rub off
- A sore that hasn’t healed after more than 14 days
- A lump, bump, or area of thickened tissue
- Unexplained bleeding in the mouth
- Numbness or tingling in a localized area
- A tooth that feels loose without clear cause
- A noticeable change in denture fit
- Difficulty swallowing, chewing, or moving the tongue
- Hoarseness or voice changes lasting more than 2 weeks
- Unexplained weight loss
What to Expect During a Dental Evaluation
If you visit your dentist with a non-healing sore, they’ll start with a full oral examination. This includes a visual inspection of all soft tissues including the tongue, gums, cheeks, and roof and floor of the mouth.
They will also palpate the area and surrounding lymph nodes, review your medical history, medications, and systemic risk factors, and take photographs or radiographs if needed. If the lesion appears suspicious, you may be referred to an oral pathologist or oral surgeon. In some cases, a small sample may be taken during an oral biopsy, typically under local anesthesia. The process is quick and relatively painless.
Understanding the Biopsy Results: What Do They Mean?
Biopsy reports are categorized in several ways. A reactive or inflammatory report often links to trauma, infection, or irritation, and is treated by removing the source of the problem.
If the results indicate dysplasia, this means there are abnormal cells that may turn cancerous if left untreated. Regular monitoring or surgical excision may be recommended.
A diagnosis of malignancy confirms cancer (usually squamous cell carcinoma), which will require further imaging and surgical planning, and may also involve chemotherapy or radiation.
Even if your biopsy comes back benign, you’ll likely be scheduled for follow-up oral care visits to monitor healing and ensure recurrence doesn’t occur.
Treatment Options: How Is a Persistent Mouth Sore Treated?
Once the cause is identified, treatment varies. Your dentist may smooth or restore a sharp tooth edge or crown, adjust or remake dentures to eliminate irritation, or prescribe antifungal or antiviral medications for infection.
If an autoimmune condition is suspected, you may be referred for medical management. Surgically removing a precancerous lesion under local anesthesia is often effective. Healing time depends on the diagnosis and treatment. Most benign lesions resolve fully within two to four weeks once the cause is addressed.
How Often Should You Check Your Mouth?
Everyone—especially smokers, alcohol users, and those over 40—should perform a self-exam monthly. Use a mirror and good lighting to inspect your cheeks, gums, lips, and tongue. Look for changes in color, texture, or shape.
Dentists recommend a professional check-up every six months, or sooner if you notice a mouth sore that won’t heal.
Final Thoughts: Don’t Wait, Just Check
A small sore can feel like no big deal—until it is. Oral cancer has one of the highest survival rates when caught early, but one of the lowest when found late.
If it’s been more than two weeks and your sore still hasn’t healed, make the call.
Frequently Asked Questions (FAQs)
- How long should a mouth sore take to heal? Most minor mouth sores caused by trauma or irritation heal within 7 to 14 days. If a sore lasts longer than two weeks, it should be evaluated by a dentist.
- Are mouth sores always painful if they are serious? No. In fact, many precancerous or cancerous lesions are painless in their early stages. That’s why it’s critical to monitor any sore that persists, even if it doesn’t hurt.
- Can stress cause mouth sores? Yes. Emotional stress, along with fatigue and hormonal changes, can trigger canker sores or worsen existing lesions, especially in those prone to ulcers.
- Is a white patch in the mouth always a sign of cancer? No. White patches (leukoplakia) can be caused by friction, fungal infections, or tobacco use. However, some may be precancerous and should be evaluated.
- Do mouth sores spread from one person to another? Some can, like cold sores caused by herpes simplex virus. Others, like canker sores or trauma-induced ulcers, are not contagious.
- What does a biopsy of a mouth sore involve? A dentist or oral surgeon numbs the area and removes a small tissue sample for laboratory analysis. It usually takes just a few minutes and has minimal discomfort.
- Are there any over-the-counter treatments for mouth sores? Yes. Antimicrobial rinses, numbing gels, and barrier pastes can help relieve symptoms. However, if a sore doesn’t heal, OTC remedies are not a substitute for diagnosis.
- Can nutritional deficiencies really cause mouth sores? Absolutely. Deficiencies in iron, vitamin B12, and folic acid can lead to recurrent ulcers and impaired healing of the oral mucosa.
- Does smoking affect healing in the mouth? Yes. Smoking irritates oral tissues, reduces blood flow, and impairs healing. It is also a major risk factor for oral cancer and precancerous changes.
- What are the risks of ignoring a mouth sore? Delaying diagnosis could allow a serious condition like oral cancer to progress. Early detection improves survival and often reduces the need for aggressive treatment.
- Can dental appliances cause persistent sores? Yes. Ill-fitting dentures, braces, or sharp crowns can create chronic trauma leading to sores that don’t heal until the appliance is adjusted or replaced.
- Is it possible to prevent mouth sores? Some can be prevented with good oral hygiene, a balanced diet, protective dental devices, and avoiding known triggers like smoking or acidic foods.
- What role does hydration play in oral health? Staying well-hydrated supports healthy mucosal tissue and helps prevent irritation and dryness that can lead to mouth sores.
- Should children be evaluated for persistent mouth sores too? Yes. While less common, chronic lesions in children can still signal infections, trauma, or systemic conditions and should not be ignored.
- What specialist should I see for a non-healing mouth sore? Start with your general dentist. If needed, they will refer you to an oral medicine specialist, oral pathologist, or head and neck surgeon for further evaluation.
The appointment you book today could make all the difference tomorrow.For patient-centered care, trusted dental screening, and compassionate support, visit Instadontics.com — where your oral health is our mission.
Keep reading: Is it a mouth sore or Something More? 10 Early Signs of Oral Cancer You Should Never Ignore