What Is Dry Mouth After Radiation?
Dry mouth after radiation, medically referred to as radiation-induced xerostomia, is one of the most common and persistent side effects experienced by individuals who undergo radiation therapy to the head and neck. It is not a minor inconvenience or a cosmetic concern. Saliva plays a central role in maintaining oral health, aiding digestion, enabling speech, supporting taste perception, and protecting the mouth from infection. When radiation damages the salivary glands, these essential functions are disrupted, sometimes permanently.
Radiation-induced dry mouth can begin early in treatment and may continue long after therapy has ended. For some people, it improves gradually over time, while for others it becomes a lifelong condition requiring continuous management.
Why Radiation Therapy Causes Dry Mouth
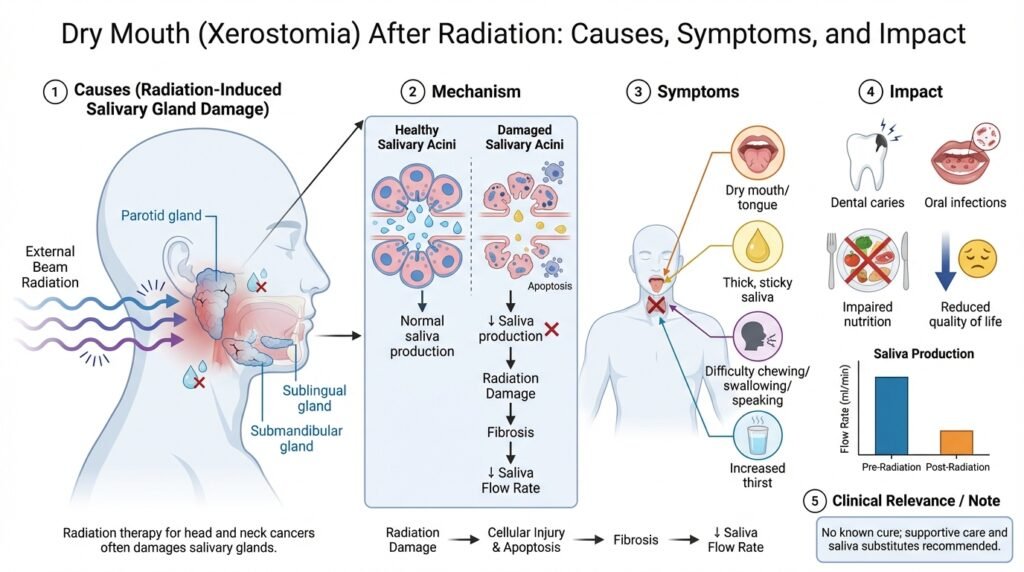
Radiation therapy works by damaging the DNA of cancer cells, preventing them from dividing and surviving. However, radiation cannot selectively target only cancerous tissue. In head and neck cancers, the salivary glands are often located within or near the radiation field, making them highly vulnerable to injury.
The major salivary glands, including the parotid, submandibular, and sublingual glands, contain specialized cells called acinar cells that produce saliva. These cells are particularly sensitive to radiation. Exposure leads to inflammation, reduced blood supply, fibrosis, and direct cellular destruction. Unlike skin or mucosal tissue, salivary glands have a limited ability to regenerate, which explains why dry mouth can persist long after radiation ends.
Salivary output often decreases significantly within the first few weeks of treatment. By the end of radiation therapy, many patients experience a severe reduction in saliva production, sometimes producing less than half of normal levels.
Changes in Saliva Quality After Radiation
Radiation affects not only the quantity of saliva but also its quality. Normal saliva is watery, protective, and rich in minerals and antimicrobial proteins. After radiation, the remaining saliva often becomes thick, sticky, and acidic. This altered saliva provides far less protection against tooth decay, infection, and tissue irritation.
The loss of saliva’s buffering ability allows acids to remain in contact with teeth for longer periods, accelerating enamel breakdown. Reduced lubrication also increases friction within the mouth, making speaking, chewing, and swallowing more difficult and uncomfortable.
Common Symptoms of Radiation-Induced Dry Mouth
Dry mouth after radiation presents with a range of symptoms that extend beyond a simple feeling of thirst. Many people describe a constant sensation of dryness or stickiness in the mouth that does not improve with drinking water. Swallowing dry or solid foods may become difficult, requiring frequent sips of liquid during meals.
Speech can feel tiring or strained as the tongue and oral tissues lack lubrication. Taste changes are common, with some patients experiencing diminished or altered taste that reduces appetite and enjoyment of food. Sleep disruption is also frequent, as individuals may wake repeatedly at night due to oral dryness, leading to chronic fatigue.
Oral tissues may appear thin, red, or fragile, and small irritations can develop into painful sores. Denture wearers often struggle with discomfort, poor fit, and ulceration due to increased friction.

Impact on Oral Health and Teeth
One of the most serious consequences of radiation-induced dry mouth is its effect on dental health. Saliva is the mouth’s primary defense against cavities. When salivary flow is reduced, acids produced by oral bacteria are not neutralized effectively, and teeth become highly susceptible to decay.
Radiation-related cavities often develop rapidly and in unusual locations, such as along the gumline or on smooth tooth surfaces that are typically resistant to decay. These cavities can progress quickly, leading to tooth fracture or loss if not addressed early.
Gum health is also affected. Reduced saliva allows plaque to accumulate more easily, increasing the risk of gingivitis and periodontal disease. In patients who have received radiation to the jaw, dental extractions pose an additional risk of osteoradionecrosis, a serious condition in which irradiated bone fails to heal properly.
Increased Risk of Oral Infections
Dry mouth creates an environment that favors the growth of harmful microorganisms. Oral fungal infections, particularly candidiasis or thrush, are common after radiation. These infections may cause burning sensations, soreness, altered taste, and red or white patches in the mouth.
Bacterial infections can also occur more easily when saliva’s antimicrobial function is compromised. Recurrent infections may become a chronic issue if dry mouth is not effectively managed.
How Long Dry Mouth Lasts After Radiation
The duration and severity of dry mouth after radiation vary widely. During treatment, symptoms typically worsen progressively. In the months following radiation, some individuals experience partial recovery as inflammation decreases and remaining salivary tissue adapts.
Modern radiation techniques, such as intensity-modulated radiation therapy, can reduce damage by sparing parts of the salivary glands when possible. However, recovery is unpredictable. Some people regain enough saliva to manage comfortably, while others experience long-term or permanent dryness.
Severity is influenced by radiation dose, size of the treatment field, whether both sides of the neck were treated, use of chemotherapy, age, smoking status, and underlying medical conditions.
Managing Dry Mouth After Radiation
Management focuses on relieving symptoms, protecting oral tissues, and preventing complications. While there is no guaranteed way to fully restore salivary gland function after severe radiation damage, a combination of strategies can significantly improve quality of life.
Frequent hydration helps temporarily, but water alone cannot replace saliva’s protective functions. Saliva substitutes and oral moisturizers are often recommended because they coat oral tissues and provide longer-lasting relief than water alone. These products do not stimulate saliva production but can reduce friction and discomfort.
For individuals with remaining salivary function, stimulation strategies may help. Sugar-free chewing gum or lozenges can encourage saliva flow, and prescription medications may be considered under medical supervision. These medications require functioning gland tissue and may cause systemic side effects, so they are not appropriate for everyone.
Diet and Lifestyle Considerations
Dietary choices can significantly influence comfort and oral health. Dry, acidic, spicy, or crumbly foods often worsen symptoms, while soft, moist foods are easier to tolerate. Adding sauces or gravies can make swallowing easier. Alcohol and caffeine can increase dryness and should be limited when possible.
Sugary foods and drinks are particularly harmful in the setting of dry mouth due to the elevated risk of cavities. Careful dietary planning is essential to maintain both nutrition and oral health.
Importance of Fluoride and Preventive Dental Care
Fluoride plays a critical role in protecting teeth after radiation. Daily use of prescription-strength fluoride significantly reduces the risk of rapid tooth decay. For many patients with chronic dry mouth, fluoride therapy is not optional but essential for long-term oral preservation.
Regular dental follow-up with professionals experienced in post-radiation care is crucial. Preventive care is far safer and more effective than restorative treatment in irradiated tissues, where healing capacity is reduced.
Emotional and Social Impact of Chronic Dry Mouth
Dry mouth affects more than physical comfort. Persistent oral discomfort can interfere with social interactions, confidence, and enjoyment of daily activities. Some individuals avoid speaking for long periods or eating in public due to embarrassment or fear of discomfort.
Recognizing and addressing the emotional impact of dry mouth is an important part of comprehensive care. Support, education, and realistic expectations can help reduce isolation and frustration.
Emerging and Supportive Therapies
Advances in radiation planning have already reduced the severity of dry mouth for many patients. Research into regenerative therapies, stem cell approaches, and salivary gland protection continues, though these options are not yet widely available.
Complementary approaches such as acupuncture have shown modest benefits for some individuals and may be considered as part of a multidisciplinary management plan when appropriate.
When to Seek Further Medical or Dental Evaluation
Dry mouth after radiation should never be ignored. Persistent pain, difficulty swallowing, weight loss, frequent infections, or rapidly developing cavities indicate that current management may be inadequate. Early evaluation allows for adjustment of care strategies and prevention of serious complications.
Living Long-Term With Dry Mouth After Radiation
For many cancer survivors, dry mouth becomes a long-term condition that requires ongoing adaptation. While complete recovery of salivary function is not always possible, effective management can preserve oral health, improve comfort, and support overall well-being.
Dry mouth is not merely a side effect to endure. It affects nutrition, communication, sleep, and quality of life. Treating it as a central component of post-radiation care, rather than a secondary concern, can make a profound difference for those living with its effects.