When we think of tooth discoloration, most people imagine the yellowing caused by coffee, tea, or smoking. However, not all stains sit on the surface of the enamel. Some discolorations are embedded deep within the tooth itself — these are known as intrinsic stains.
Unlike surface (extrinsic) stains, intrinsic stains are notoriously harder to treat and often require more than a simple whitening toothpaste or professional cleaning. In this comprehensive review, we will delve deep into:
- What intrinsic stains are
- Their causes
- How they differ from extrinsic stains
- Diagnostic approaches
- Available treatment options
- Preventative strategies
- Future research and advancements
Let’s dive in.
What Are Intrinsic Stains?
Intrinsic stains occur within the tooth structure, either in the enamel (the outermost layer) or more commonly, the dentin (the layer beneath the enamel). These stains result from changes in the tooth’s internal composition or damage that causes discoloration from within.
In simple terms, while extrinsic stains are like dirt on a window, intrinsic stains are like fog inside the glass.
Key Characteristics:
- Location: Inside enamel or dentin
- Appearance: Gray, brown, yellow, or even blue hues
- Response to Whitening: Poorer compared to surface stains
- Persistence: Long-term unless treated professionally
Causes of Intrinsic Tooth Stains
There are several causes, often related to events that affect the tooth during its development or after it has matured. Let’s break them down:
1. Developmental Causes
- Fluorosis:
Excessive fluoride intake during enamel formation (childhood) can cause white spots, mottling, or brown patches. - Tetracycline Antibiotics:
If tetracycline or its derivatives are taken during tooth development (e.g., in pregnancy or early childhood), it can bind to calcium ions in the teeth, causing gray, yellow, or brown bands. - Genetic Conditions:
Conditions such as amelogenesis imperfecta (defective enamel) and dentinogenesis imperfecta (defective dentin) lead to teeth that are discolored from the moment they erupt.
2. Post-Developmental Causes
- Trauma:
Injury to a developing or mature tooth can cause internal bleeding, leading to a darkened or gray tooth. - Pulp Necrosis:
Death of the pulp (the innermost tissue containing nerves and blood vessels) often results in discoloration. - Dental Restorations:
Materials like amalgam can leach and cause dark stains within the surrounding tooth structure. - Aging:
Over time, enamel thins and dentin darkens, giving the teeth a more yellowed or brownish appearance. - Internal Resorption:
A pathological process where the tooth structure is resorbed from the inside, leading to pinkish staining (“pink tooth of Mummery”).
Intrinsic vs. Extrinsic Stains
To fully appreciate intrinsic stains, it’s important to differentiate them clearly from extrinsic stains:
| Feature | Intrinsic Stains | Extrinsic Stains |
|---|---|---|
| Location | Within enamel or dentin | On the surface (enamel) |
| Causes | Developmental issues, trauma, medications, aging | Food, beverages, tobacco, poor hygiene |
| Treatment | Bleaching, bonding, veneers | Cleaning, surface whitening |
| Color | Gray, brown, yellow, blue | Yellow, brown, black |
| Ease of Removal | Difficult | Easier with cleanings and whitening |
Diagnosing Intrinsic Stains
Proper diagnosis is key to selecting the correct treatment. Here’s how dentists approach it:
- Clinical Examination:
- Assess color, location, and distribution of stains
- Check for history of trauma, medication use, or systemic conditions
- Radiographs (X-rays):
- Evaluate for pulp necrosis, internal resorption, or previous dental work
- Transillumination:
- Using a bright light to examine the internal structures for variations in opacity
- Patient History:
- Asking about childhood illnesses, antibiotic use, fluoride exposure, and past injuries
Treatment Options for Intrinsic Stains
Since intrinsic stains are internal, treatment options differ significantly from those for extrinsic stains.
1. Internal Bleaching
Reserved for non-vital (root canal-treated) teeth.
- Process:
- Access cavity created
- Bleaching agent (like sodium perborate) placed inside
- Sealed temporarily
- May require several sessions
- Best for:
- Single dark tooth post-trauma or root canal
2. External Bleaching
Sometimes external bleaching agents can penetrate enamel and lighten mild intrinsic stains.
- Techniques:
- In-office bleaching (higher concentration agents)
- At-home bleaching kits (lower concentration, longer duration)
- Limitations:
- Less effective for deep tetracycline or fluorosis stains
3. Microabrasion
Useful for superficial intrinsic discolorations.
- Process:
- Application of acidic and abrasive agents to remove a thin enamel layer
- Indications:
- Mild fluorosis, superficial stains
4. Composite Bonding
Masking the stain with composite resin material.
- Advantages:
- Minimally invasive
- Immediate results
- Disadvantages:
- May stain over time
- Requires maintenance
5. Porcelain Veneers
Thin shells of porcelain bonded to the front of teeth.
- Best for:
- Severe intrinsic discolorations unresponsive to bleaching
- Pros:
- Highly esthetic
- Long-lasting
- Cons:
- Requires tooth reduction
- Higher cost
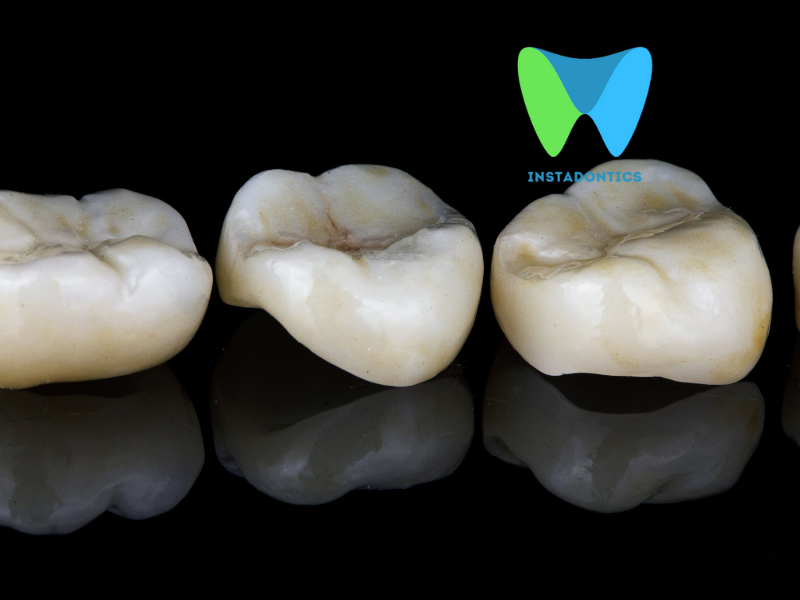
6. Full Coverage Crowns
Used for extensive discolorations, especially when the tooth is also structurally compromised.
- Considerations:
- More invasive
- Best reserved for teeth needing structural reinforcement
Preventing Intrinsic Stains
While not all intrinsic stains are preventable, several strategies can minimize risks:
- Limit Fluoride Intake:
- Monitor fluoride levels in water and avoid excessive supplements in children
- Avoid Tetracycline in Pregnancy and Young Children:
- Use alternative antibiotics when necessary
- Prevent Trauma:
- Use mouthguards during sports
- Educate children about dental safety
- Good Oral Hygiene:
- Regular dental checkups to monitor developing teeth
- Prompt Treatment of Dental Injuries:
- Immediate care after trauma can reduce chances of internal discoloration
Future Trends and Research
The treatment of intrinsic stains is a dynamic field, and research is ongoing to find better solutions. Promising areas include:
- Nanotechnology-Based Whitening Agents:
- Aim for deeper penetration with reduced sensitivity
- Biomimetic Materials:
- New resins and ceramics that better mimic natural enamel’s appearance and light properties
- Enamel Regeneration:
- Research into materials that can actually rebuild enamel instead of masking defects
- Genetic Therapies:
- Early-stage research suggests potential to correct some developmental discolorations at the genetic level (e.g., amelogenesis imperfecta)
Intrinsic tooth stains represent one of the most challenging cosmetic dental issues. Their internal nature makes them resistant to traditional whitening treatments, and each case must be evaluated individually. While prevention remains the best strategy whenever possible, today’s advancements in bleaching, bonding, veneers, and crowns provide patients with multiple avenues to restore a bright, confident smile.
Key takeaways:
- Not all discolorations are created equal — intrinsic stains demand a deeper understanding.
- Diagnosis is crucial: history, clinical exam, and imaging are essential.
- Treatment must be customized: What works for one patient may not work for another.
- New technologies offer hope for even better and less invasive options in the future.
For anyone struggling with discolored teeth, a consultation with an experienced dentist who understands the complexities of intrinsic staining is essential. There is almost always a way to significantly improve the appearance of your smile — it just might require a little more care, expertise, and creativity.
Intrinsic Teeth Stains: Frequently Asked Questions (FAQs)
1. What are intrinsic stains?
Intrinsic stains are discolorations that occur inside the tooth structure (the dentin), rather than on the surface (enamel). These stains are often deeper and harder to remove than surface (extrinsic) stains.
2. What causes intrinsic stains?
Common causes include:
- Medications (e.g., tetracycline antibiotics taken during childhood)
- Excessive fluoride during tooth development (fluorosis)
- Tooth trauma (injury can cause a tooth to darken)
- Genetic conditions affecting tooth color
- Aging (dentin naturally yellows over time and enamel thins)
3. How are intrinsic stains different from extrinsic stains?
- Intrinsic stains: Located inside the tooth, harder to remove, often require professional treatment.
- Extrinsic stains: On the tooth surface, caused by foods, drinks, or smoking, often removable with cleaning or whitening toothpaste.
4. Can intrinsic stains be removed by whitening toothpaste or professional cleaning?
No, whitening toothpastes and regular dental cleanings are generally not effective for intrinsic stains, as these treatments only address surface discoloration.
5. What are the treatment options for intrinsic stains?
- Professional teeth whitening (bleaching): Sometimes effective, especially for mild cases.
- Internal bleaching: Used for teeth that have darkened after root canal treatment.
- Dental bonding: Tooth-colored resin is applied to cover the stain.
- Porcelain veneers or crowns: Thin shells or caps placed over the tooth to mask discoloration.
6. Are intrinsic stains dangerous to my health?
No, intrinsic stains are usually a cosmetic issue and do not typically indicate a health problem, unless caused by trauma or decay.
7. Can children get intrinsic stains?
Yes. Children are especially at risk if they take certain medications (like tetracycline) or are exposed to too much fluoride while their permanent teeth are developing.
8. Can intrinsic stains be prevented?
- Avoid giving children tetracycline antibiotics during tooth development.
- Use appropriate fluoride levels (consult your dentist).
- Protect teeth from injury.
- Maintain good oral hygiene to prevent decay that can lead to discoloration.
9. How do I know if my stain is intrinsic or extrinsic?
Intrinsic stains are usually:
- Gray, blue, or brown in color
- Uniform throughout the tooth or in bands
- Resistant to regular cleaning and whitening
Your dentist can help diagnose the type of stain and recommend the best treatment.
10. Will over-the-counter whitening products help with intrinsic stains?
Most OTC whitening products are not very effective for intrinsic stains. Stronger, dentist-supervised treatments may be needed.
11. Is there any risk to whitening treatments for intrinsic stains?
Professional whitening is generally safe when supervised by a dentist, but overuse or improper use of whitening agents can cause tooth sensitivity or gum irritation.
12. Should I see a dentist for intrinsic stains?
Yes! Intrinsic stains often require professional assessment and treatment. Your dentist can recommend the safest and most effective options for improving your smile.
If you notice persistent or unusual discoloration of your teeth, consult your dentist for an accurate diagnosis and personalized treatment plan.