Rheumatoid arthritis (RA) and periodontal disease (gum disease) are two chronic inflammatory conditions that can significantly impact an individual’s health and quality of life. While they affect different systems in the body—joints and oral health, respectively—emerging research highlights a notable connection between the two. This blog explores the relationship between rheumatoid arthritis and periodontal disease, examining their shared risk factors, symptoms, and implications for treatment.
What is Rheumatoid Arthritis?
Rheumatoid arthritis is an autoimmune disorder characterized by chronic inflammation of the joints. The immune system mistakenly attacks the synovium, the lining of the membranes that surround the joints, leading to pain, swelling, and eventual joint damage. RA can also have systemic effects, affecting other tissues and organs in the body.
Key Symptoms of Rheumatoid Arthritis
- Joint pain and stiffness, particularly in the morning or after periods of inactivity
- Swelling and tenderness in the joints
- Fatigue and malaise
- Fever and weight loss
- In severe cases, joint deformities
What is Periodontal Disease?
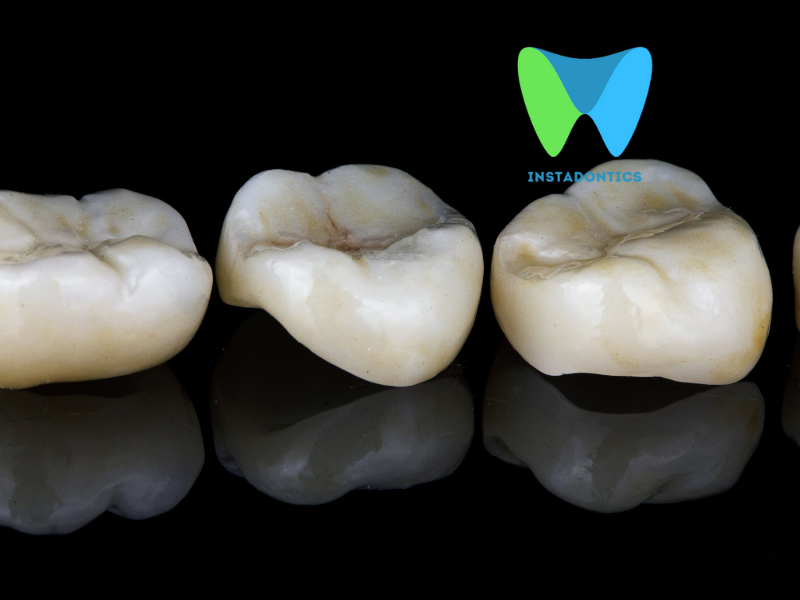
Periodontal disease is an inflammatory condition affecting the tissues that support the teeth, primarily caused by plaque buildup. It begins with gingivitis, characterized by inflammation and bleeding of the gums, and can progress to periodontitis, which involves the destruction of the supporting structures of the teeth, including bone.
Key Symptoms of Periodontal Disease
- Red, swollen, or bleeding gums
- Persistent bad breath
- Receding gums
- Loose teeth or changes in bite alignment
- Pain when chewing
The Connection Between Rheumatoid Arthritis and Periodontal Disease
1. Shared Inflammatory Pathways
Both rheumatoid arthritis and periodontal disease are characterized by chronic inflammation. Research indicates that the inflammatory cytokines involved in RA, such as tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6), are also present in periodontal disease. This overlap suggests that individuals with RA may experience heightened inflammation in their gums, increasing their susceptibility to gum disease.
2. Increased Risk of Periodontal Disease in RA Patients
Studies have shown that individuals with rheumatoid arthritis are at a higher risk of developing periodontal disease. A systematic review published in the Journal of Clinical Periodontology found that the prevalence of periodontal disease was significantly higher in RA patients compared to those without the condition. The inflammation associated with RA can compromise the health of the gums, making them more vulnerable to infection.
3. Impact of Gum Disease on Rheumatoid Arthritis
Conversely, gum disease can exacerbate the symptoms of rheumatoid arthritis. The chronic inflammation resulting from periodontal disease can enter the bloodstream, potentially worsening systemic inflammation and joint pain. A study published in Clinical Oral Investigations demonstrated that RA patients with periodontal disease reported higher levels of pain and disability compared to those without gum disease.
Oral Manifestations of Rheumatoid Arthritis
Rheumatoid arthritis can manifest in various ways within the oral cavity, including:
- Dry Mouth (Xerostomia): Medications used to manage RA, such as antihistamines and opioids, can lead to reduced saliva production, increasing the risk of cavities and gum disease.
- Gingival Inflammation: The inflammatory response in RA can extend to the gums, resulting in swollen and bleeding gums.
- Temporomandibular Joint (TMJ) Disorders: RA can affect the TMJ, leading to pain, limited movement, and difficulty chewing.
Treatment Implications
1. Integrated Healthcare Approach
Given the interconnectedness of rheumatoid arthritis and periodontal disease, an integrated healthcare approach is crucial. Patients with RA should be encouraged to maintain regular dental check-ups and communicate openly with their dental professionals about their condition. Conversely, dentists should be aware of the patient’s rheumatoid arthritis status when assessing oral health.
2. Managing Gum Disease
For individuals with rheumatoid arthritis, managing gum disease is essential for overall health. Effective oral hygiene practices, including brushing twice daily, flossing, and using antibacterial mouthwash, can help prevent gum disease. Regular professional cleanings are also crucial for maintaining gum health.
3. Medication Considerations
Certain medications used to treat rheumatoid arthritis, such as methotrexate, can have side effects that impact oral health. Methotrexate has been associated with gum recession and increased risk of periodontal disease. Patients should discuss potential side effects with their healthcare providers and ensure they receive appropriate dental care.
4. Treating Periodontal Disease
For individuals with both RA and gum disease, treating periodontal disease may lead to improvements in RA symptoms. Some studies suggest that managing gum disease can help reduce systemic inflammation, potentially alleviating joint pain and stiffness. This highlights the importance of a comprehensive treatment plan that addresses both conditions.
Related: Best Supplements for Gum Health
The relationship between rheumatoid arthritis and periodontal disease is complex and multifaceted, underscoring the need for an integrated approach to healthcare. As research continues to uncover the connections between these two conditions, it is clear that managing oral health is essential for individuals with rheumatoid arthritis. By prioritizing dental care, maintaining good oral hygiene, and fostering communication between healthcare providers, patients can improve their overall health outcomes and quality of life.
In summary, understanding the interplay between rheumatoid arthritis and periodontal disease can empower patients to take proactive steps in managing their health. Regular dental visits, effective oral hygiene practices, and a collaborative approach to treatment can significantly enhance the well-being of those affected by these chronic conditions.